Dental
How To Measure Your RCM Success
February 25, 2023
Paul Chen
Use algorithms to process the image and extract important features from it
Convallis in vel aliquam in et semper adipiscing tincidunt sapien ac placerat malesuada sed netus orci duis sit tristique nec condimentum amet morbi malesuada ut enim purus ultricies nec commodo nunc condimentum neque non sodales sem lacus quis sit in diam nisl dolor morbi habitant hendrerit laoreet ornare lectus nulla eget elementum sit ullamcorper suspendisse malesuada neque lectus tortor amet.
Use machine learning to classify the image into different categories
Aliquam dictumst in rhoncus facilisi odio eleifend egestas non elit tempus imperdiet scelerisque magna nullam eget etiam et ante purus et ligula euismod mi lectus quam varius leo fermentum vitae curabitur pretium habitant et duis maecenas.
- Lorem ipsum dolor sit amet consectetur non sodales sem lacus
- Mauris aliquet faucibus iaculis dui vitae ullamco
- Euismod mi lectus mauris aliquet faucibus iaculis dui vitae ullamco
- Posuere enim mi pharetra neque proin dic facilisi odio

Filter the images based on a variety of criteria, such as color, texture, and keywords
Risus nullam neque ac imperdiet eu. Suspendisse nisi placerat rutrum aenean consectetur bibendum viverra aliquam. Nunc venenatis platea eu id porttitor felis bibendum nulla quam. Viverra facilisis phasellus massa risus amet. Dolor sit bibendum aliquet neque nam mattis nisi ut sed. Est in elementum id.
“Vitae proin leo cras risus eget tellus quam convallis mauris fermentum magna imperdiet nullam tincidunt luctus porttitor purus elementum eget”
Automatically group similar images together and apply a common label across them
Risus nullam neque ac imperdiet eu. Suspendisse nisi placerat rutrum aenean consectetur bibendum viverra aliquam. Nunc venenatis platea eu id porttitor felis bibendum nulla quam. Viverra facilisis phasellus massa risus amet.
- Lorem ipsum dolor sit amet consectetur morbi lorem vel lorem
- Mauris aliquet faucibus iaculis dui vitae ullamco
- Posuere enim mi pharetra neque proin dic platea eu id porttitor
- Pellentesque massa posuere enim mi pharetra neque proin dic lorem
Convert the extracted features into a vector representation of the image
Semper nunc ut leo iaculis. Quis sit eget urna nibh fringilla accumsan ac morbi est vulputate vestibulum montes mauris ridiculus vulputate vitae cursus. Sed id urna ornare ultrices non in. Sit egestas aliquet id sit morbi lorem vel lorem venenatis sed pellentesque non vitae cursus scelerisque nulla ut proin sed mattis nulla lorem pellentesque massa mattis sed tempor condimentum id pellentesque imperdiet nam.
We frequently have conversations with DSOs about revenue cycle performance, metrics, and KPIs. The dental revenue cycle generates mass amounts of useful data which can sometimes seem overwhelming and difficult to organize. However, if you believe the noted management consultant Peter Drucker who said, “You can’t improve what you don’t measure,” then where and how do you start? For any DSO, starting with these five baseline metrics is a great foundation to find simplicity on the other side of complexity. Data is your friend.
Percentage of A/R Greater than 90 Days
Aged receivables exist in every DSO and practice. Calculating the % of receivables over 90 days is an important indicator of the overall health of your RCM because, while some claim failures are inevitable, too high a percentage in the 90 day plus range can be a sign of more systematic and serious resourcing or billing challenges. It’s human nature to deal with the easy claims first, but allowing an unpaid claim to age drastically reduces the chance of receiving any payment at all. Even if the balance is ultimately transferred to the patient, patients will struggle to remember and not feel compelled to pay for a procedure months after a visit. This metric is becoming increasingly more important as out-of-pocket costs rise, so keep a close eye on it.
Ideally, less than 15% of your receivables should reach this age, but the lower the better. The cost to collect increases over time, and the longer you allow your accounts to age, the less likely it is you will recover them and the more it will cost you to do so.
Clean Claim Rate
An ounce of prevention is worth a pound of cure. A clean claim is a claim that flows from submission to collection without needing additional involvement from the RCM team after the first submission. Clean Claim Rate gives your team visibility to problems that are causing claims to require resubmissions, like mistakes in patient registration information or claims failing to meet a payer’s requirements.
They say, “you never have time to do it right, but you always have time to do it over.” Slow down, and focus on clean submissions, clean claims is the #1 way to reduce revenue cycle workload and increase collection speed, the best groups average over 70% in clean claims.
Collection Days
Collecting what is owed entirely and quickly is what all RCM teams aspire to. Tracking your collection days, the difference between the payment date and date of service, can help you improve your cash flow by identifying and fixing problems in your billing and collections processes that are causing delays in payment. By reducing your collection days you increase the amount of money you collect in a given time period, which can have a significant impact on your overall cash flow. For example, if you are able to reduce your collection days by 10 days and you collect an average of $100,000 per day, you’ve increased your cash flow by $1,000,000.
Ideally, you want to be able to turn over your A/R in less than 30 days. Top performing teams can collect open A/R in less than 15 days though this metric will vary by payer mix as well.
Denial Rate
Your denial rate is the percentage of insurance claims that are fully denied by the payers. There are a couple of possible variations to this metric as it can be calculated both at the claim level but also at the claim line level. Let’s focus on the claim level. This metric validates the effectiveness of your pre-billing processes, especially your insurance eligibility and benefit validation process. A low denial rate indicates that your revenue cycle processes are working well and you are preventing as many mistakes from happening as possible. Keeping an eye on this metric could alert you to claim pre-billing verification opportunities, submission issues, or sometimes credentialing issues that could dramatically affect your revenue and cash flow.
The best performers have an average claim denial rate below 5%, but many DSOs and practices are regularly over 10%.
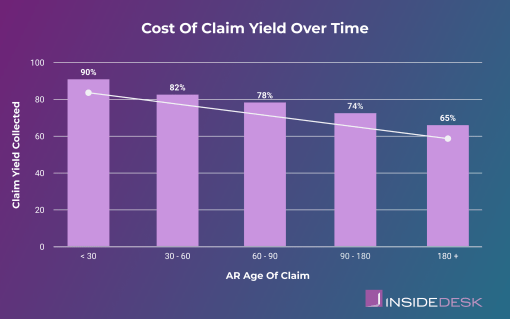
Claim Yield
The final baseline metric your practice should be regularly monitoring is Claim Yield. This measure represents what the payer paid against the expected fees. For example, if your practice collected 70 claims with a total expected amount of $10,000 and received only $6,000 in payer payment, then the claim yield would be 60%.
A high claim yield indicates that the organization is able to successfully collect payment for a large percentage of the claims it submits. On the other hand, a low claim yield may be a sign of problems with the organization’s billing and collections processes, such as incorrect coding, inadequate follow-up on unpaid claims, incorrect fee schedule, or other issues that may be causing claims to be denied. By tracking claim yield and identifying areas for improvement, organizations can optimize their billing and collections processes and increase their overall revenue.
Ideally, every claim you submit for payment would be paid at 100% but we know that isn’t the case. Best practices dictate that your Claim Yield should be greater than 90%, industry best performers can achieve up to 95%.
Starting with a solid understanding of these five key metrics will give you confidence troubleshooting, allocating your time and resources, and put you and your RCM team on a path to continuous improvement. Monitoring them consistently over time will help ensure that your RCM results are stable, reliable, and hopefully optimized.